A recent study published in the journal Clinical Psychology & Psychotherapy has established a clear link between excessive daydreaming, which disrupts daily life, and difficulties managing emotions among individuals with borderline personality disorder (BPD) and depression. This type of daydreaming, known as maladaptive daydreaming, may function as an avoidance strategy for coping with overwhelming emotions.
Borderline personality disorder is a severe mental health condition characterized by profound shifts in mood, behaviour, and self-perception. Individuals with BPD often struggle with prolonged feelings of anger, sadness, or anxiety and face challenges in maintaining stable relationships due to a deep fear of abandonment and intense interpersonal dynamics.
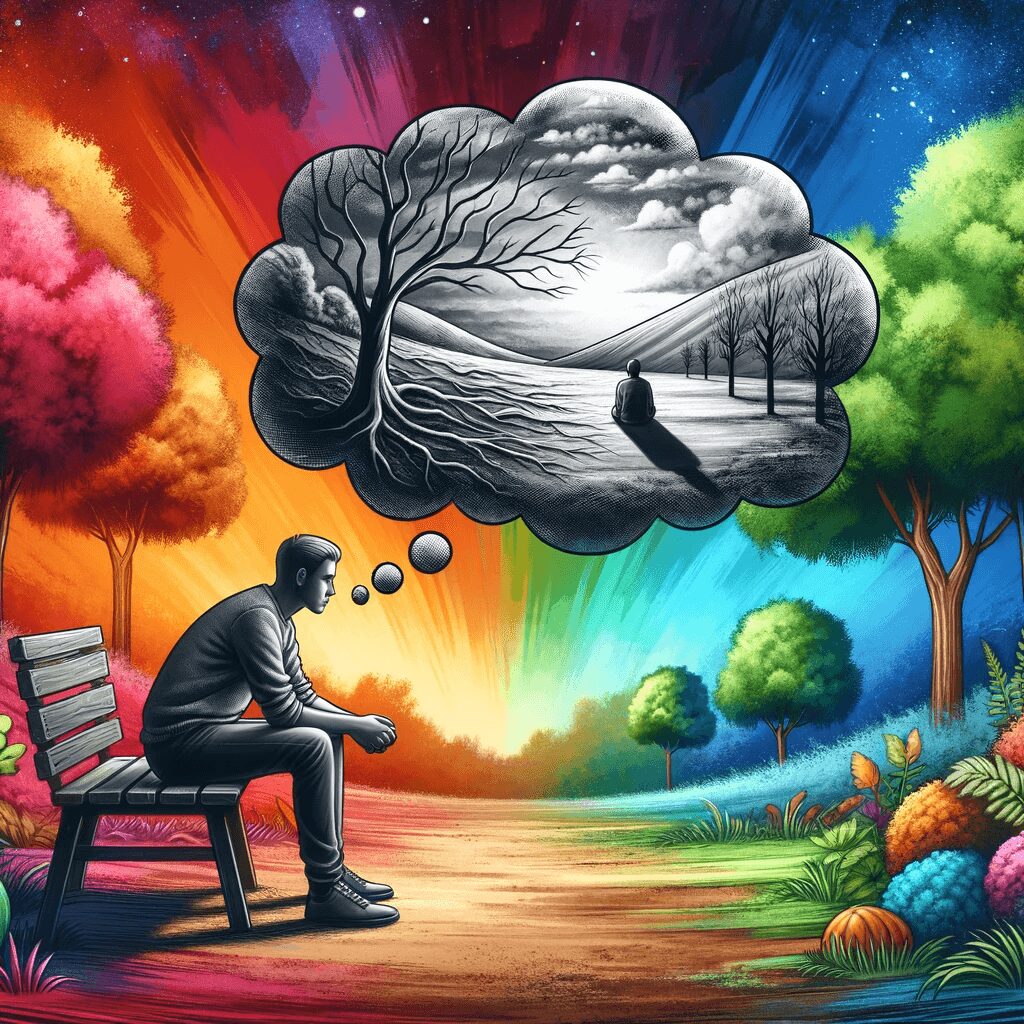
Maladaptive daydreaming involves immersive fantasies that significantly interfere with a person’s ability to function in daily life, potentially leading to neglect of relationships, work, or education. It becomes an escape from reality.
Prior to this study, little attention had been given to how maladaptive daydreaming relates to BPD, despite its known associations with other mental health issues. The researchers aimed to investigate whether individuals with BPD utilize daydreaming as a coping mechanism for intense emotions.
The study involved 188 participants, including 102 individuals with BPD and 86 with depression. The findings revealed that those with BPD experienced greater difficulty managing their emotions and exhibited higher levels of self-stigmatization compared to those with depression. Both groups engaged in harmful daydreaming, but the BPD group utilized daydreaming more as an escape from distressing emotions.
Individuals with BPD reported stronger negative emotions such as sadness or anger compared to the depression group. The study also identified connections between maladaptive daydreaming and the desire to escape reality, as well as between emotional struggles and self-stigmatization.
In light of these findings, the study suggests that Dialectical Behavior Therapy (DBT) could be an effective intervention for individuals with BPD who struggle with maladaptive daydreaming. DBT equips individuals with the skills to manage intense emotions and live more mindfully. It encompasses techniques such as mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
For instance, mindfulness practices can help individuals stay present in the moment and avoid getting lost in harmful daydreams. Distress tolerance skills can provide alternatives to daydreaming during times of distress. Emotion regulation techniques can assist in understanding and controlling overwhelming feelings, while interpersonal effectiveness training can enhance healthy communication and relationship-building.
While this study provides essential insights, it is crucial to acknowledge its limitations. The majority of participants were women, raising uncertainty about the generalizability of the findings. Future research should engage directly with participants to gain deeper insights into their specific symptoms and their relationship to maladaptive daydreaming.
The study titled “Maladaptive daydreaming, emotional dysregulation, affect, and internalized stigma in persons with borderline personality disorder and depression disorder: A network analysis,” authored by Anna Pyszkowska, Julia Celban, Ari Nowacki, and Izabela Dubiel, highlights the need for targeted interventions addressing maladaptive daydreaming in individuals with BPD.