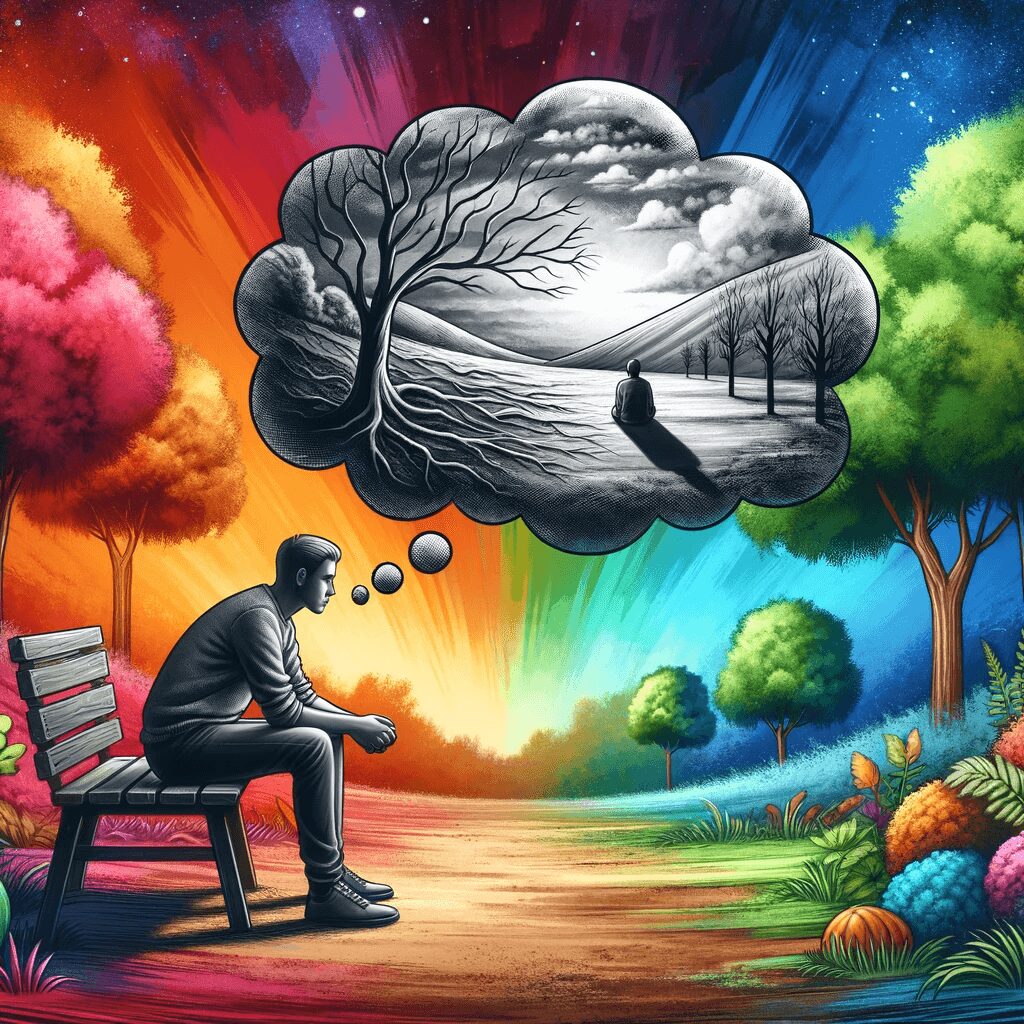
People with Borderline Personality Disorder (BPD) often face immense emotional pain, and in their struggle to cope, they may resort to non-suicidal self-injury (NSSI) behaviours. These acts are not intended to be fatal but instead serve as a means of dealing with overwhelming emotions or gaining control. This article explores the various NSSI behaviours adopted by individuals with BPD and the factors contributing to their development.
- Cutting
Cutting is one of the most common forms of NSSI among individuals with BPD. Using a sharp object like a knife, razor, or scissors, the individual cut their skin, often on the arms, legs, or stomach. The act of cutting is believed to provide temporary relief from emotional pain and generate feelings of control or release. It is essential to recognize that cutting is a maladaptive coping mechanism and is often a cry for help.
- Burning
Burning is another prevalent form of NSSI. It involves intentionally causing burns to the skin using various methods like cigarettes, lighters, or heated objects. Like cutting, burning can provide a sense of relief from overwhelming emotions, albeit momentarily. It can also lead to scarring and infection, emphasizing the need for appropriate intervention and support.
- Scratching and Picking
Some individuals with BPD may excessively scratch or pick their skin, hair, or nails. This behaviour, also known as dermatillomania or excoriation disorder, is a form of NSSI that can lead to scarring, infection, and a perpetuation of the cycle of self-harm.
- Biting
Biting is another NSSI behaviour in which individuals bite themselves, often breaking the skin and causing bruising. This method of self-harm can result in infections, scarring, and emotional distress.
- Hitting or Banging
Individuals with BPD may deliberately hit or bang their bodies against hard surfaces, such as walls or furniture, as a form of NSSI. This behaviour can lead to bruising, fractures, and other injuries. It serves a similar purpose as other NSSI behaviours: coping with overwhelming emotions and regaining a sense of control.
Factors Contributing to NSSI in BPD
- Emotional Dysregulation
A hallmark feature of BPD is emotional dysregulation, or the inability to effectively manage and respond to emotional experiences. Individuals with BPD often have intense, overwhelming emotions that they struggle to understand and control. NSSI behaviours can provide a temporary release from these emotions or serve as a distraction.
- Impulsivity
Impulsivity is another characteristic of BPD, leading individuals to act on their emotions and urges without considering the consequences. This impulsivity can contribute to adopting NSSI behaviours to cope with difficult emotions.
- Invalidating Environment
An invalidating environment in which an individual’s emotional experiences are dismissed or criticized can exacerbate the symptoms of BPD and contribute to developing NSSI behaviours. Invalidation can lead to feelings of worthlessness and intensify emotional pain, which may prompt NSSI as a coping mechanism.
- History of Trauma
Many individuals with BPD have a history of trauma, such as abuse or neglect. Traumatic experiences can contribute to the development of BPD and the adoption of NSSI behaviours to cope with unresolved pain and feelings of worthlessness.
Treatment and Support
Recognizing and addressing NSSI behaviours in individuals with BPD is crucial to provide the necessary support and treatment. Some effective treatment options for BPD and NSSI behaviours include:
- Dialectical Behavior Therapy (DBT)
DBT is a specialized form of cognitive-behavioural therapy (CBT) that teaches individuals with BPD how to regulate their emotions, tolerate distress, and build healthier interpersonal relationships. DBT has been proven to be highly effective in reducing NSSI behaviours and improving overall functioning.
- Mentalization-Based Therapy (MBT)
MBT is a psychodynamic therapy that aims to enhance an individual’s capacity to understand their own and others’ mental states, which can help improve emotional regulation and reduce NSSI behaviours. MBT helps individuals with BPD develop healthier coping strategies and build stronger relationships.
- Schema Therapy
Schema therapy is an integrative therapeutic approach that combines elements of CBT, psychodynamic therapy, and attachment theory. It focuses on identifying and modifying maladaptive schemas, or deeply ingrained patterns of thinking and behaviour, that contribute to BPD symptoms and NSSI behaviours.
- Medication
While there are no specific medications for BPD, certain psychiatric medications can help manage the symptoms contributing to NSSI behaviours. Antidepressants, mood stabilizers, and antipsychotics may be prescribed to target emotional dysregulation, impulsivity, and other related issues.
- Support Networks
Building a strong support network is crucial for individuals with BPD navigating their recovery journey. Family, friends, therapists, and support groups can provide encouragement, understanding, and guidance, helping individuals develop healthier coping strategies and reduce their reliance on NSSI behaviours.
Non-suicidal self-injury behaviours are a complex and dangerous coping mechanism many individuals with Borderline Personality Disorder use to deal with overwhelming emotions. By understanding the various forms of NSSI and the factors contributing to their development, we can better support those struggling with BPD and encourage healthier coping strategies. Treatment options like DBT can help individuals develop the skills and support necessary to overcome NSSI behaviours and lead healthier, more fulfilling life.