Introduction
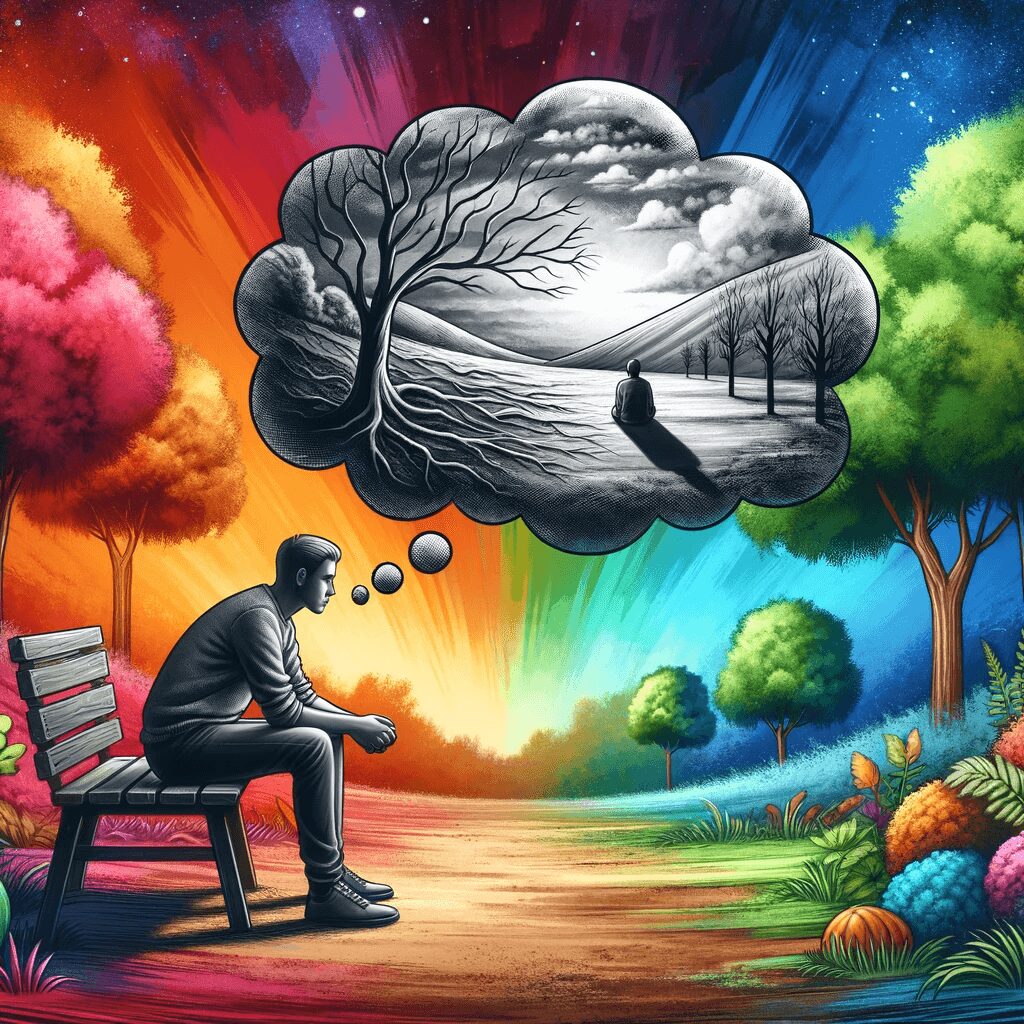
Non-suicidal self-injury (NSSI) is prevalent among individuals diagnosed with borderline personality disorder (BPD). NSSI refers to intentionally injuring one’s body without suicidal intent, such as cutting, burning, or hitting oneself. It mainly concerns the potential for serious physical harm and the risk of developing suicidal behaviour.
This article will discuss how clients with BPD use NSSI as short-term coping mechanisms and explore effective prevention strategies from dialectical behaviour therapy (DBT) and acceptance and commitment therapy (ACT). These therapeutic approaches can support individuals seeking healthier ways to manage their emotional pain.
The Role of NSSI in BPD
BPD is a complex mental health disorder characterized by unstable relationships, intense emotions, impulsivity, identity disturbance, and recurrent self-harm behaviours like NSSI. For those with BPD, NSSI often serves to regulate overwhelming emotions or cope with distressing experiences.
There are several reasons why individuals with BPD engage in NSSI:
- Emotion Regulation: People with BPD may use self-injury to regulate intense emotions. By focusing on the physical sensation of pain or seeing blood, they temporarily distract themselves from emotional suffering.
- Self-Punishment: Some individuals with BPD may view self-injury as punishment for perceived shortcomings or feelings of unworthiness.
- Communication: In some cases, people who engage in NSSI do so to express their emotional pain non-verbally or elicit care from others.
- Control: When an individual feels that their life is spiralling out of control due to emotional turmoil, NSSI can control their body and pain.
- Grounding: Self-injury can help individuals with BPD feel more connected to reality when they experience dissociation, a common symptom in this population.
Dialectical Behavior Therapy (DBT)
DBT is an evidence-based treatment specifically developed for individuals with BPD. This therapy combines cognitive-behavioural techniques with mindfulness practices to address the core issues contributing to self-destructive behaviours like NSSI. DBT focuses on four main modules: mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness.
Mindfulness
Mindfulness involves non-judgmental awareness of the present moment. By practicing mindfulness, clients can develop greater self-awareness and learn to recognize triggers for NSSI. For example, clients might become aware of the emotions and thoughts that arise before engaging in self-injury and use this information to intervene earlier.
Emotion Regulation
Emotion regulation skills aim to help clients better understand their emotions and develop healthier ways to manage them. Clients learn to identify emotions, reduce vulnerability factors for negative emotions, increase positive experiences, and use coping strategies like opposite action or problem-solving.
Distress Tolerance
Distress tolerance skills focus on helping clients tolerate overwhelming situations without resorting to self-destructive behaviours like NSSI. Techniques include distraction (engaging in pleasurable activities), self-soothing (using comforting items or activities), improving moment-to-moment awareness through grounding exercises, and radical acceptance.
Interpersonal Effectiveness
Interpersonal effectiveness teaches clients how to effectively communicate their needs and boundaries while maintaining self-respect and enhancing relationships. This can help reduce the likelihood of engaging in NSSI as a means of communication or to elicit care from others. Skills taught include assertiveness, empathic listening, and conflict resolution.
Acceptance and Commitment Therapy (ACT)
ACT is another therapeutic approach found compelling for individuals with BPD. Although not explicitly designed for this population, its principles can help clients manage their emotional distress and reduce reliance on NSSI as a coping mechanism. The core processes of ACT are acceptance, cognitive defusion, being present, self as context, values clarification, and committed action.
Acceptance
Acceptance involves embracing one’s thoughts and feelings without judgment or attempts to change them. This helps clients develop a healthier relationship with their internal experiences instead of struggling against them – a struggle that often leads to NSSI.
Cognitive Defusion
Cognitive defusion aims to change how clients relate to their thoughts rather than changing the content itself. Techniques like distancing oneself from unhelpful thoughts or observing thoughts as passing events can help prevent these thoughts from triggering self-destructive behaviours like NSSI.
Being Present
Like mindfulness in DBT, being present in ACT focuses on non-judgmental awareness of the here and now. By grounding themselves in the present moment, clients can become more aware of triggers for NSSI and intervene before engaging in self-injury.
Self as Context
In ACT, the concept of self as context refers to recognizing one’s ongoing sense of self that remains constant despite ever-changing emotions and experiences. This process helps clients understand that they are more than their symptoms or self-destructive behaviours like NSSI.
Values Clarification
Values clarification involves identifying one’s core values – what is truly important in life – and using these values to guide decisions and actions. By clarifying what matters most to them, clients can direct their energy towards more fulfilling activities instead of engaging in self-injury.
Committed Action
Committed action entails making commitments to take steps towards valued goals and persisting in facing obstacles. By focusing on meaningful actions aligned with personal values, clients can create a sense of purpose that reduces the need for NSSI as a coping mechanism.
Wrap up
NSSI is a complex behaviour often used by individuals with borderline personality disorder as a short-term coping skill to manage intense emotions and distress. Dialectical behaviour therapy (DBT) and acceptance and commitment therapy (ACT) offer valuable strategies to prevent NSSI by teaching clients healthier ways to regulate emotions, tolerate distress, and create a fulfilling life aligned with their values. Through these therapeutic approaches, individuals with BPD can develop the skills to reduce reliance on self-destructive behaviours and build more satisfying lives free from self-injury.