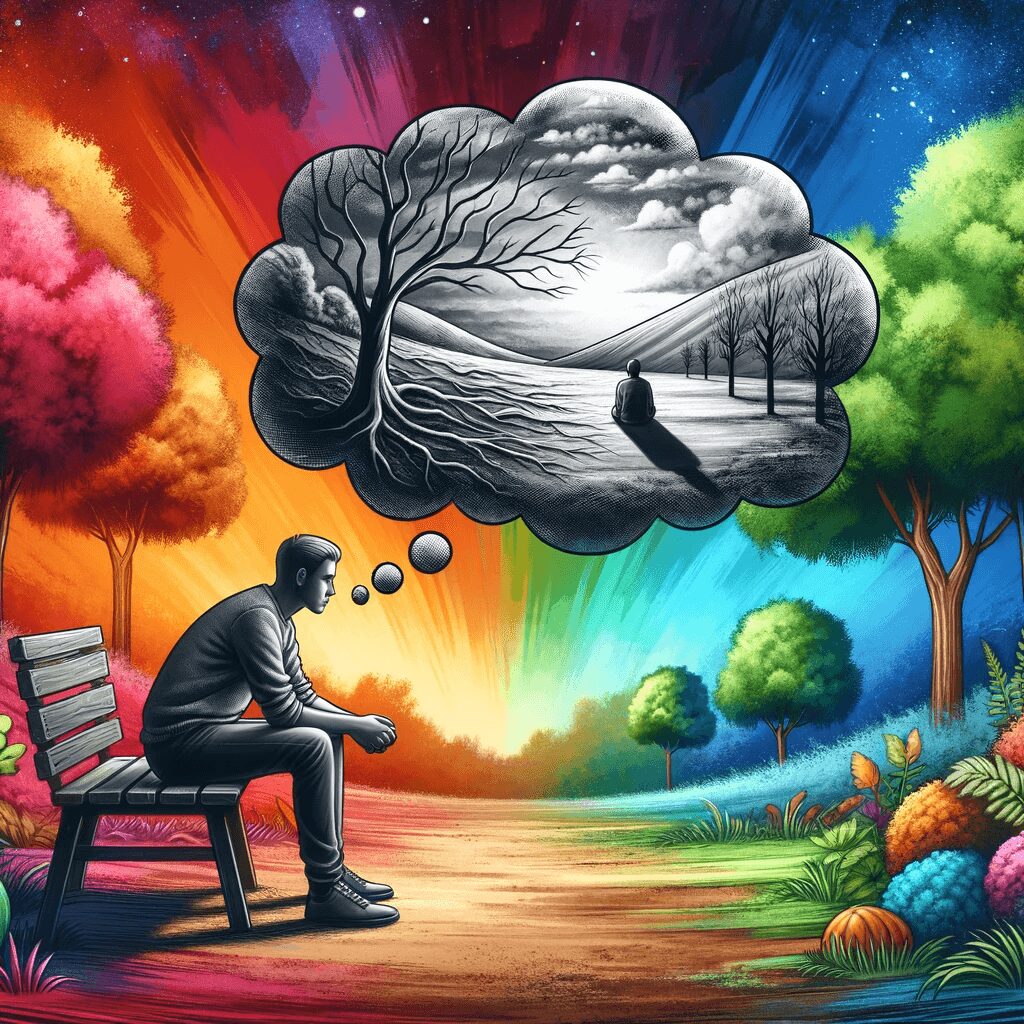
Quiet Borderline Personality Disorder (Quiet BPD) is a less understood and often overlooked subtype of Borderline Personality Disorder (BPD). It’s characterized by similar patterns of unstable emotions, relationships, and sense of self as BPD but differs in its outward expression. Individuals with Quiet BPD often internalize their struggles, making it challenging for others, and even themselves, to recognize their disorder.
Symptoms and Features of Quiet Borderline Personality Disorder
Like traditional BPD, quiet BPD is marked by emotional instability, identity issues, and turbulent relationships. However, the critical distinction lies in how these symptoms are manifested.
Emotional Instability
People with Quiet BPD experience intense emotions like those with classic BPD. However, instead of acting out, they direct these feelings inward. They may struggle with feelings of emptiness, self-loathing, and extreme sadness.
Turbulent Relationships
While individuals with classic BPD may have tumultuous relationships, those with Quiet BPD are more likely to withdraw. They may harbour an intense fear of abandonment and, as a result, become overly compliant or self-sacrificing in relationships.
Issues with Identity
A distorted sense of self is common in Quiet BPD. These individuals may have difficulty understanding who they are and what they want, leading to feeling lost or misunderstood.
Quiet Borderline Personality Disorder vs. Traditional Borderline Personality Disorder
The distinguishing factor between traditional BPD and Quiet BPD is how the symptoms are expressed. Traditional BPD symptoms are more visible, with individuals often engaging in impulsive behaviours and having visible mood swings. On the other hand, those with Quiet BPD internalize their symptoms, often appearing calm and composed on the outside.
Causes of Quiet Borderline Personality Disorder
Although the exact cause of Quiet BPD is unknown, a combination of genetic predisposition, environmental factors, and brain structure abnormalities may contribute to its development. Childhood trauma, such as physical, emotional, or sexual abuse, may also play a significant role.
Diagnosis and Treatment of Quiet Borderline Personality Disorder
Diagnosing Quiet BPD can be complex due to its internalized symptoms. Mental health professionals rely on detailed medical histories, psychological evaluations, and diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Once diagnosed, treatment for Quiet BPD may involve psychotherapy, medication, and self-care strategies. Dialectical Behavior Therapy (DBT) is often recommended, focusing on teaching coping skills to manage intense emotions and improve relationships.
Coping with Quiet Borderline Personality Disorder
Living with Quiet BPD can be challenging, but it’s essential to remember that help is available. Joining a support group, maintaining a healthy lifestyle, and sticking to a treatment plan can significantly improve the quality of life.
Validity of the Quiet Borderline Personality Disorder Diagnosis
The validity of the Quiet BPD diagnosis has been debated in the psychiatric community. As it stands, Quiet BPD is not officially recognized as a distinct subtype in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the primary resource used by mental health professionals for diagnosis. However, many professionals and individuals affected by the condition strongly identify with “Quiet BPD.” They argue that it accurately describes symptoms not fully captured by the traditional BPD diagnosis. Despite the lack of formal recognition, Quiet BPD is increasingly used in clinical settings, highlighting the need for further research and a potential re-evaluation of the current diagnostic criteria.