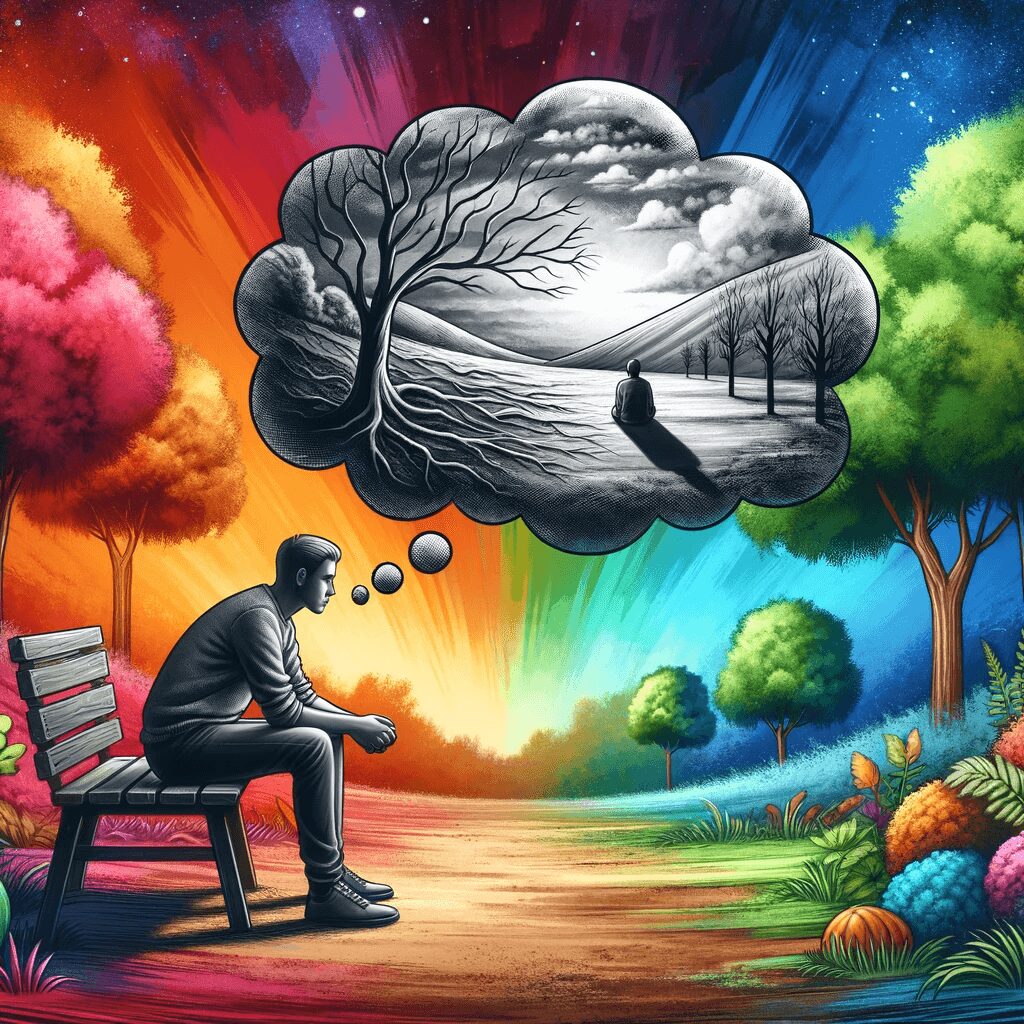
Borderline Personality Disorder (BPD) is a complex mental health condition that can significantly impact a person’s life. Unstable moods, an unstable sense of self, relationship difficulties, and a fear of abandonment characterize it. One common experience associated with BPD is anxiety, which often co-occurs with the disorder. Understanding the relationship between BPD and anxiety is crucial for effective diagnosis and treatment. This article will explore the connection between BPD and anxiety, the prevalence of comorbidities, and the challenges in diagnosing and treating these conditions.
What is Borderline Personality Disorder?
Borderline Personality Disorder is one of the ten personality disorders recognized by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Individuals with BPD often experience rapidly shifting, unstable moods, an unstable sense of self, and difficulty maintaining stable relationships. They may engage in black-and-white thinking and exhibit impulsive behaviours. BPD is also associated with an increased risk of self-harm and suicide.
The Prevalence of Borderline Personality Disorder
Borderline Personality Disorder affects approximately 1.4% of the population in the United States. It is important to note that BPD often co-occurs with other mental health disorders. Studies have shown that 84.7% of individuals with BPD have one or more additional mental health disorders. This high rate of comorbidity makes it challenging to diagnose and treat BPD effectively.
The Link Between BPD and Anxiety
Anxiety is a common comorbidity in individuals with BPD. The intense emotional dysregulation experienced by individuals with BPD can contribute to heightened anxiety, fear, and stress. Additionally, individuals with BPD often struggle with interpersonal relationships, leading to social anxiety and difficulties in social functioning.
Comorbidities of BPD
In addition to anxiety, individuals with BPD may have other comorbid mental health disorders. Some of the most common comorbidities include:
– Bipolar Disorder
Bipolar disorder often co-occurs with BPD, with up to 20% of individuals with bipolar disorder also meeting the criteria for BPD. Both disorders share symptoms of emotional dysregulation and impulsive behaviour, making it challenging to differentiate between them.
– Post-Traumatic Stress Disorder (PTSD)
PTSD is another comorbidity frequently seen in individuals with BPD. Traumatic experiences like childhood abuse can increase the risk of developing both conditions. Early childhood trauma may alter the brain and increase the likelihood of developing BPD and PTSD.
– Major Depressive Disorder
Major depressive disorder is a mood disorder that commonly co-occurs with BPD. Symptoms of depression, such as low mood, lack of interest, and sleep problems, may overlap with BPD symptoms. However, individuals with BPD experience emotional dysregulation and difficulties in interpersonal relationships, distinguishing it from major depressive disorder.
– Substance Use Disorder
Due to impulsivity, individuals with BPD are at a higher risk of developing a substance use disorder. Substance use can temporarily alleviate emotional distress, making it a coping mechanism for individuals with BPD. It is estimated that up to 72% of individuals with BPD will also develop a substance use disorder at some point.
– Eating Disorders
Eating disorders, such as anorexia, bulimia, and eating disorders not otherwise specified (EDNOS), frequently co-occur with BPD. These disorders may develop as individuals with BPD attempt to regulate their emotions through disordered eating behaviours. Approximately 90% of individuals with BPD meet the criteria for an eating disorder.
– Other Personality Disorders
While it is rare for individuals to be diagnosed with multiple personality disorders, exhibiting traits of other personality disorders alongside BPD is possible. These personality disorders include paranoid personality disorder, schizoid personality disorder, schizotypal personality disorder, antisocial personality disorder, histrionic personality disorder, narcissistic personality disorder, avoidant personality disorder, dependent personality disorder, and obsessive-compulsive personality disorder.
Challenges in Diagnosis and Treatment
Diagnosing BPD and its comorbidities can be challenging due to overlapping symptoms and its associated stigma. Clinicians may be reluctant to diagnose BPD due to the stigma surrounding the condition. Additionally, the heterogeneity of BPD symptoms and the varying severity among individuals can complicate the diagnosis process.
To increase the chances of an accurate diagnosis, finding a clinician who conducts a comprehensive evaluation, including a structured interview, is essential. This evaluation should assess current and past symptoms and consider the individual’s thought processes, relationships, and self-perception.
Treatment for BPD and its comorbidities often involves a combination of psychotherapy and, in some cases, medication. Dialectical Behavior Therapy (DBT) is one of the most effective therapies for BPD, helping individuals regulate their emotions and manage impulsive behaviours. However, not all individuals can access DBT programs, and alternative therapies, such as cognitive-behavioral therapy (CBT), may be beneficial. It is crucial to seek professional support and find the right treatment approach based on individual needs.
Conclusion
Understanding the relationship between Borderline Personality Disorder and anxiety is essential for accurate diagnosis and effective treatment. Individuals with BPD often experience high anxiety levels due to emotional dysregulation and difficulties in interpersonal relationships. BPD frequently co-occurs with other mental health disorders, such as bipolar disorder, PTSD, major depressive disorder, substance use disorders, eating disorders, and other personality disorders.
Diagnosing BPD and its comorbidities can be challenging due to overlapping symptoms and stigma. Seeking a comprehensive evaluation from a qualified clinician is crucial for accurate diagnosis and treatment planning. Psychotherapy, particularly DBT, is the gold standard for BPD treatment, but alternative approaches may also be effective. With proper diagnosis and treatment, individuals with BPD and comorbid anxiety can achieve improved mental well-being and quality of life.