Borderline Personality Disorder (BPD) is a multifaceted psychological disorder affecting millions globally. The commonly recognized symptoms of BPD include emotional instability and impulsivity. However, there exists a lesser-known subtype known as “Quiet BPD,” which is chiefly characterized by inward struggles and the propensity to repress emotions instead of expressing them externally. In this discourse, we’ll penetrate into the subtleties of Quiet BPD, delving into the notions of overcontrol and undercontrol, which are often associated with it.
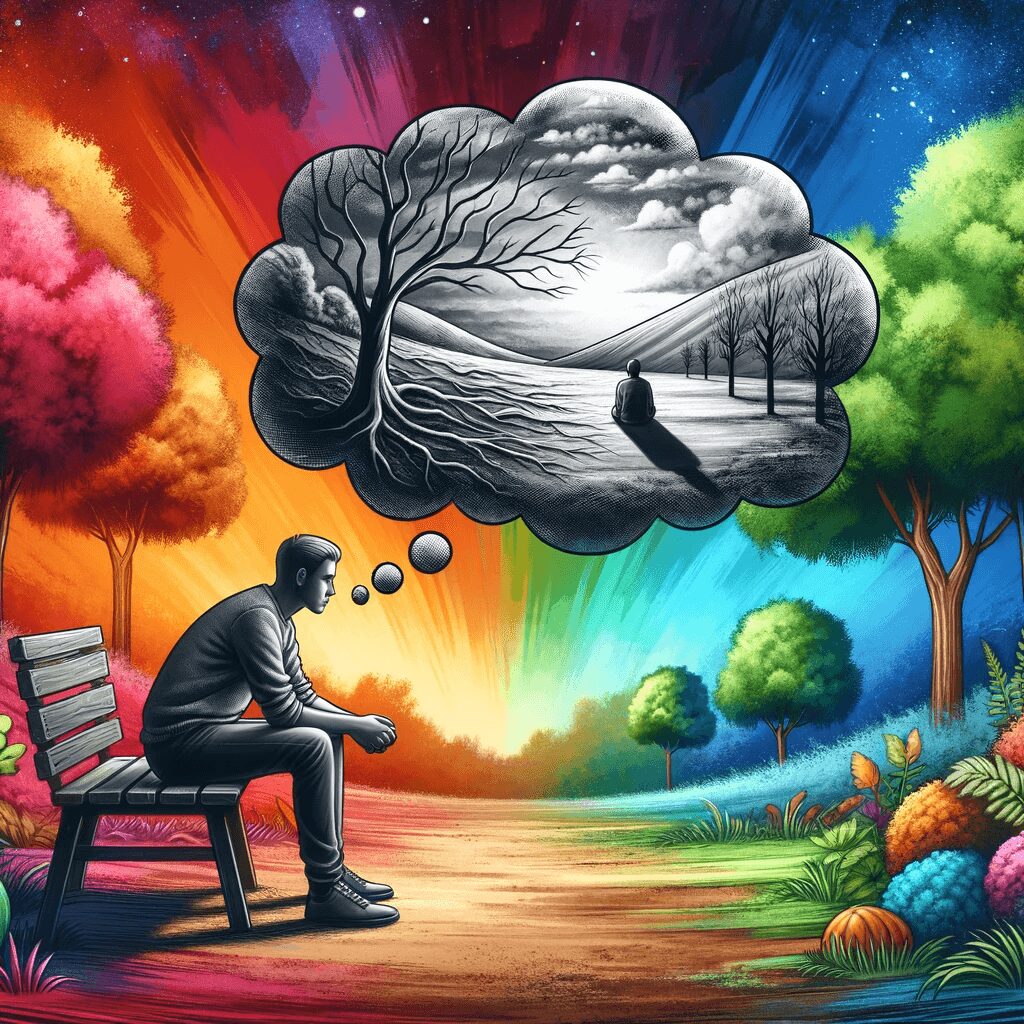
“Quiet BPD,” also referred to as “High-Functioning BPD” or “Emotionally Unstable Personality Disorder,” is an informal version of BPD. It’s defined by emotion internalization, an outwardly composed demeanour, and the stifling of explicit signs of emotional stress. Individuals suffering from Quiet BPD might grapple with severe internal emotional tumult but find it challenging to communicate these feelings to others, leading to feelings of seclusion and bewilderment.
It is important to note that Quiet BPD is not recognized as an official subtype in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition-TR (DSM-5TR). The DSM-5TR, published by the American Psychiatric Association, is a widely used guide for classifying and diagnosing mental health disorders. While the DSM-5TR includes the diagnostic criteria for Borderline Personality Disorder (BPD), it does not explicitly recognize Quiet BPD as a separate subtype. However, it is worth mentioning that the DSM-5TR acknowledges the heterogeneity and variability of BPD presentations, highlighting that individuals with BPD may exhibit a range of symptoms and coping mechanisms, including internalized emotions and the suppression of outward expressions. The term “Quiet BPD” has emerged within clinical and research contexts to describe a distinct presentation of BPD characterized by internalizing emotions. Still, its official recognition as a diagnostic subtype within the DSM-5TR is currently lacking.
Overcontrol: The Battle Within
Overcontrol is a phenomenon intimately tied to Quiet BPD. It relates to an overbearing pattern of self-control and emotional inhibition exhibited by individuals struggling with Quiet BPD. Fears such as appearing vulnerable or imposing their emotions on others may lead these individuals towards perfectionism, extreme self-reliance, and suppressing their emotions for a semblance of control.
The aspect of overcontrol in Quiet BPD can trigger numerous challenges. It can hamper personal relationships due to an inherent fear of emotional intimacy and hesitance in seeking help—thus distancing close ones. Furthermore, overcontrol can contribute to consistent feelings of emptiness and dissatisfaction since these individuals might rob themselves of authentic emotional connections and satisfaction.
Undercontrol: The Unexpected Release
Even though overcontrol is primarily associated with Quiet BPD, it’s important not to overlook instances where undercontrol could come into play for individuals grappling with it. Undercontrol signifies scenarios where they struggle to contain their emotions precisely – resulting in outbursts or impulsive behaviours that appear out of place for them.
Such episodes could arise due to accumulated pressure from suppressed emotions that eventually need an outlet. This contradictory mixture of overcontrolling yet sometimes undercontrolling behaviour makes the experience particularly tough for those dealing with Quiet BPD; they swing between stifling their emotions and sudden inundations of overpowering feelings.
Treatment and Support
Addressing Quiet BDP requires a holistic approach focusing on both tendencies towards overcontrolling or undercontrolling behaviours. Psychotherapy–particularly Dialectical Behavior Therapy (DBT)–has proven effective in enabling individuals to cope better with their emotions, develop healthier coping mechanisms, and enhance interpersonal skills.
Support from near ones becomes quintessential here—it helps create an environment where those dealing with Quiet BD feel at ease sharing their feelings without apprehension about being judged harshly. Active listening combined with empathy and affirmation about what they’re going through can bring about significant shifts in their path toward recovery.